 Whooping cough was the last thing on my mind as we packed for a late summer vacation at the beach. But on the second day there, our baby’s cough got considerably worse…we realized that we had an insidious guest. The pertussis bacteria had traveled with us on vacation.
Whooping cough was the last thing on my mind as we packed for a late summer vacation at the beach. But on the second day there, our baby’s cough got considerably worse…we realized that we had an insidious guest. The pertussis bacteria had traveled with us on vacation.
The really scary thing is, my babe was the last of the four kids to get the “bad cough”. Up to that point, we really had only thought of it as a cold with a bad, lingering cough. We started researching based on the symptoms we’d observed with our kids, and realized that we had whooping cough. We had lived with it for a couple of months, unaware.
At the doctor’s office, my baby was smiley and didn’t seem sick at all, and (of course!) he didn’t cough once during our visit. the nurse practitioner began telling me that it didn’t seem to be croup; he seemed perplexed and a bit anxious when I asked him about whooping cough. He agreed that the symptoms fit, and told me that the Dr’s in the practice had just (as in that weekend) agreed to plan a course of action for diagnosing whooping cough (aka Pertussis) because the medical journals are beginning to call attention to the disease. He said because of the vaccines, they simply don’t consider it, but the medical journals are bringing attention back to pertussis, as it’s being grossly misdiagnosed and under-reported. I had questions, but the answers I was getting didn’t make sense to me. After our visit, I really began researching this disease in earnest.
The information I was getting from my pediatrician, the CDC, and other mainstream sources seemed contradictory to me. Some sources stated that infants under a year with whooping cough should be hospitalized (really?), but my doctors office didn’t seem that concerned. What was going on here?
I became slightly obsessed with knowing more about whooping cough, so that I could make an informed choice for treating my kids, as well as for protecting others around us from being exposed to this virulent bug. And it IS virulent…my oldest two have been vaccinated against it, and they were the first two to come down with whooping cough.
I have heard of a LOT of cases of this in the past year popping up among friends all over the U.S. I am of the opinion that the current vaccine may be failing, but I don’t think doctors are really aware of this, nor are they equipped with good diagnostic or treatment options at this point. (We’ll discuss more on this in part II)
Whooping cough hasn’t really gotten on the national radar screen. Yet.
Now, I do enjoy research, but I’m generally not obsessive about picking apart a disease in medical textbooks and sharing it with the world. Especially diseases like whooping cough…it sounded somewhat antiquated, mostly mild outbreaks, and I thought that there were easily available treatments.
But I discovered that whooping cough is extremely contagious; and it’s contagious before you even know you have it, and by the time you get to the doctor, the damage has already been done. After spending some serious reading time, I feel that in this case, it’s super-important to “know thy enemy.” Allow me to introduce you…
In a nutshell, here’s what I think every parent should be aware of in regards to whooping cough:
*People who have been immunized can still get whooping cough.
*Pertussis is most contagious when only minor cold like symptoms are present…and at that stage, it’s *extremely* contagious.
* Most cases go undiagnosed, and are uneventful…a mild persistent cough in adults and older kids (and rarely “whoops”), but the damage that whooping cough can do in young infants (under 6 months), the elderly, and those who have impaired immune systems is extremely serious and can be life threatening.
*Pertussis is often misdiagnosed or misunderstood, and incorrect information about the disease is common, even in doctors offices.
*Whooping Cough is often diagnosed after the damage is done, and is commonly overlooked as a persistent cough. Other names for it are the “100 day cough” and “nurses cough”.
Whooping Cough: Just the Facts
Whooping cough is the only vaccine-preventable disease on the rise in the US and it is severely under-reported.(2) The Center for Disease Control (CDC) estimates that, at best, one out of three cases are believed to be reported (2); but other estimates place the true number of reported incidences at closer to 1 out of 10 to 1 out of 20 reported cases. (2) Those are pretty shocking stats…or better stated, a shocking lack of stats.
Imagine the impact of this in daycare centers and schools alone.
Whooping cough can actually be caused by one of three bacteria. B. Pertussis is thought to cause 95% of the cases of whooping cough, with B Parapertussis, a milder strain, causing the other 5% of reported cases. (1)
Now, my friends, if you’re up for it, here are the cliff notes from my obsessive research plus, my own little cute illustrations, for us visual learners. From medical textbooks, lectures, and government authorities, here’s a peek into the dirty lair of the whooping cough <dun-da-dah-dunnnn>
The Stages of Whooping Cough
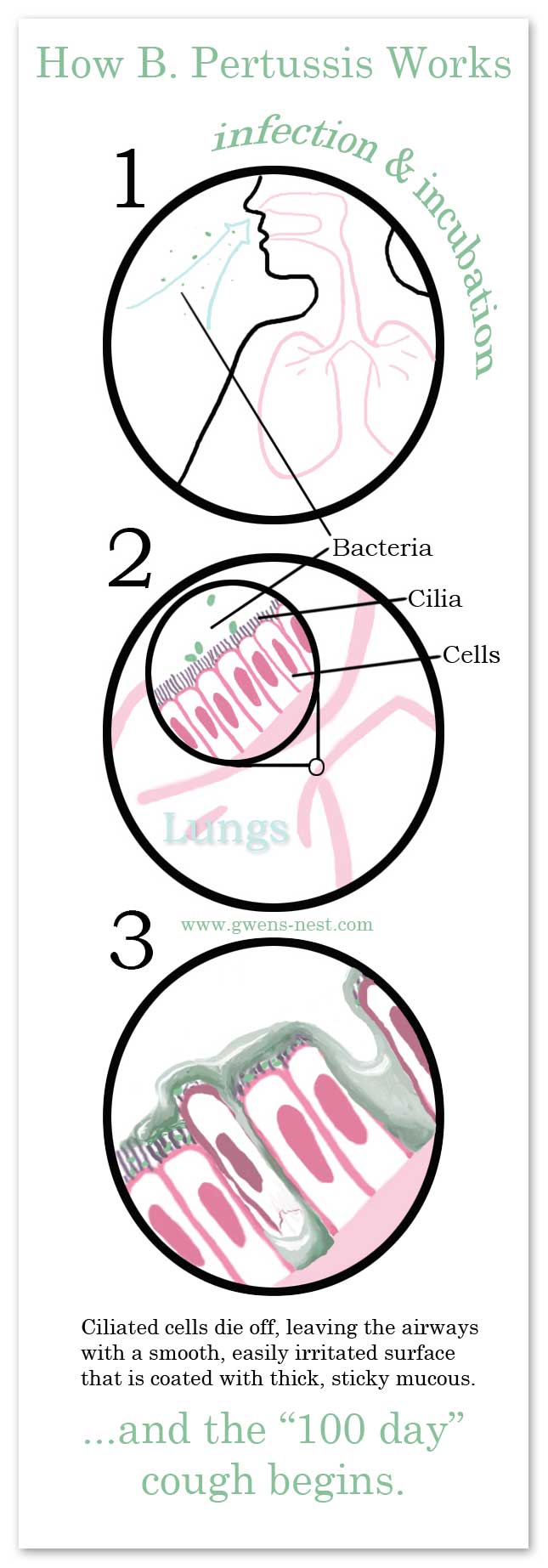
Stage One: Infection and incubation
(note: many sources roll this stage in with the second stage)
Day one: B. pertussis bacteria is inhaled and attaches itself to the mucous membranes…the infection begins. Whooping Cough is spread by breathing in the bacteria from the discharge of an infected persons cough or sneeze. (3)
Grody.
Immediately, the bacteria begins to colonize and multiply on the cells lining the respiratory tract and airways. The protective cell layer that lines the airways are like living velvet…they are covered in tiny hairs or cilia. The cilia move back and fort, expelling mucous, and tiny foreign particles, including invading bacteria. But B. pertussis is magnetically attracted to these ciliated epithelial cells. Itattaches to them and begins to silently colonize and obliterate the lining of the large airways.(4)
The incubation period lasts on average from 7-10 days, but can range from 4 to 21 days in which the person is highly contagious, but has no symptoms at all. The pertussis bacteria never actually enters the cells or the bloodstream. So sytemic or oral treatment is minimally helpful. Pertussis is very effective at causing major respiratory distress.
Stage Two: The Catarrh (Inflammation & Mucuous) Stage
For approximately the past week, these quickly multiplying bacteria are coating the upper respiratory tract, and doing massive damage to the cells that line the airways.
The infected cells are exploding, pumping out toxins that damage lining of the airways, which in turn increase histamine response and mucous production, and ramps up the immune response of the host. (3) Symptoms begin to show, but are very mild, and will mimic that of a cold, with a runny nose, mild occasional cough, and low grade fever. (4) In our cases, only one child had a fever, and the others had very, very minor cold symptoms with an occasional cough or a sniffle. In babies, this may present as sneezes and throat clearings.
As the top layer of ciliated cells die off, the body reacts with acute inflammation and by producing large amounts of thick, sticky mucous. (1) This stage goes on for one to two weeks. (2)
So, to sum up:
For three weeks or more, these buggers are stripping your airway of cilia, creating gunky thick mucous, you’re majorly contagious…and you may just have a minor sniffle.
<shudder>
I’m a visual person, so I thought I’d share a visual aid of what is happening in the first 2 phases of whooping cough.
Stage Three: The Paroxysmal (Fits) Stage
Next comes the coughing stage, which lasts from two to six weeks. This is usually when we begin to get a clue that something is very, very wrong. Most cases are diagnosed in this stage of the illness.
The person will present with violent fits of coughing, interspersed with deep gasps for air that can make a whooping sound. Though, in our four cases, only one child had the classic ‘whoop’, and only did so one time.
This is where you really begin to see the damage that has been happening to the lining of the airways. On average, the coughing fits increase in frequency during the first 1 to 2 weeks, remain at the same level for 2 to 3 weeks, decreasing gradually after this. (2)
Coughs may be hard, dry, convulsive coughs, or more croupy and rattley as mucous begins to be expelled. (6) The thick, sticky mucous is difficult to expel, and once a coughing spasm begins, it usually continues until all the air is expelled from the lungs. It is common for the person to throw up during or just after a coughing fit. (1)
The coughing spasms can also cause a person to turn red or blue in the face (cyanotic), blood vessel ruptures in the whites of the eyes, and in some cases, cracked ribs and hernias. (1)
My little ones would literally cough all the air out of their lungs until they puked. Every night, sometimes multiple times a night. For weeks.
The pertussis bacteria puts off a toxin that causes an increased histamine response, which means that the respiratory tract overreacts easily, triggering these major coughing fits.(3) The coughing spells average about 15 times in a 24 hour period, and occur most commonly at night, which results in fitful sleep (understatement of the year).(1)
Other activities such as eating or laying down can also cause coughing spells to occur. For my 6 1/2 month old, pretty much all of his normal activity triggered cough spells: rolling over, laying on his tummy, drooling, putting things in his mouth, burping, and nursing. It was heart wrenching.
The crazy thing is, between coughing fits, the person seems perfectly normal, and feels fine. Which is part of the reason why this so often goes undiagnosed…the child doesn’t look or feel sick unless they start coughing, and, of course, they never, ever have a coughing fit at the doctors’ office. In adults, whooping coughing may just seem to be a mild, persistent cough. The “whoop” is uncommon in adults. (2)
Stage Four: Recovery or convalescent phase
The final stage is the recovery period, which can take up to six months. Coughing fits begin to happen with less frequently and duration. (3) The lungs recover slowly, and the person is more susceptible to secondary infections because the protective cilia layer is gone. Infections that do develop afterwards are going to stimulate similar coughing fits.
So, now you may know more about pertussis than your average nurse practitioner. It’s some scary stuff.
I had more questions…What can be done about it? How dangerous is it, and how do you treat it?
Fear not, my friends…we’ll look at these questions and more in the very next post:
Whooping Cough II: Dangers, Diagnosis & ConventionalTreatments
Sources cited:
1. Dr. Neal R.Chamberlain, http://www.atsu.edu/faculty/chamberlain/Website/lectures/lecture/reairin2.htm
2. http://www.jabfm.org/cgi/content/full/19/6/603
Note: this study was funded by the “largest company in
the world devoted entirely to human vaccines.” Just so you know.
3. Essentials of Immunology and Serology, By Jacqueline Stanley, 2002 http://tiny.cc/n89sh
4. Bacterial Toxins and Virulence Factors In Disease by Joel Moss, 2008 http://tinyurl.com/2a5c794
5.http://www.cdc.gov/pertussis/
6. Whooping-cough; its pathology and treatment, By Thomas Michael Dolan, 1882 http://tinyurl.com/2asybrq
(obviously, very inaccurate with regards to pathology, but interesting in
regards to immunity and history of the disease)
I have read and reread your posts on whooping cough (all 3 of them) my daughter (3 1/2) has a severe case, right now we are on night 20 of the paroxysm coughing, when you said your kids coughed and threw up at night for weeks, how many weeks??? I feel like I’m at my breaking point, yesterday I just cried and cried every time she had a coughing fit (I never let her see me). I’m giving her SA to bowel tolerance and even purchased some Lypo-spheric stuff to give her at night. She’s a picky eater anyways and her appetite is Terrible anyways, so I can’t get her to eat the stew you made. I just feel like she will never be well again and it’s ripping my heart into a million pieces.
Oh, Mama…I’m so sorry. It’s so hard on everyone to go without sleep and to be on call for that long. 🙁 The nickname for whooping cough is the ‘hundred day cough’, but the coughing fits should ease in intensity.
My older kids coughed that long, but once I discovered the turmeric trick, they all started getting better MUCH faster.
If she doesn’t like the turmeric, just add more honey or maple syrup until it tastes yummy to her. Vitamin C is also great for this.
See if you can get some family support to catch some naps, and just watch her temps for secondary infection. This too shall pass. ♥ Just keep saying, “lifetime immunity”.
“People who have been immunized can still get whooping cough.
Whooping cough is the only vaccine-preventable disease on the rise in the US and it is severely under-reported.”
Aren’t those statements contradictory?
Nicki Woodard
It can be prevented by vaccination but the vaccination loses efficacy after time. So no…both of those things are true. 🙂
So, did their cough get progressively worse, or was it just a mild cough that, one day, became drastically worse? We may have been exposed and are waiting on our cultures to come back. Thanks for the info.
It seemed to get worse quickly once it started. It was worse at night for sure, and they seemed perfectly healthy between coughing fits.
Some helpful hints for whooping cough:
Boil water with cinnamon, clove, and lemon. Let it simmer on low all day long. (Be careful of course)
Elderberry syrup for coughs. Mix with juice if they won’t take it directly. (I always mix every juice with half water)
Blueberry juice has amazing antioxidants and vitamin C. However, broccoli has 4 times the amount of vitamin C than Oranges. (I use Organic in the box. Saves a LOT of time)
About your child’s eating habits: Never give your children sugar. It’s horrible for everyone of us, but doubly so for our kids. Also, no ketchup. Salt and sugar are a bad combination, and if you give them to your kid, they won’t want anything else. They satisfy cravings, and, not unlike drugs, we crave them all the more. Sure, Diabetes and other diseases occur, but more importantly, our bodies do not build immunity with sugar and salt diets. It’s been 2 weeks, and my daughter is in the healing process. She had all the symptoms of pertussis 1, 2, and is now in recovery. (yes, the throwing up and everything) But because we’re very organic based (fanatics), at 1 year and 6 months old, our little one finally succumbed to her first sickness. She’s never been sick in her life, and now we’re so glad we’ve stuck to our regimen. We don’t vaccinate, and will never inject toxins, heavy metals, animal DNA, or human embryo diploid cells into our precious girl. Immunity is built from breast feeding, organic foods, and clean water.
In addition to the above, you can also use oregano oil on feet with carrier oil ( 2 drops each). And also, Drosera can help immensely. It’s from the carnivorous plant, Drosera rotundifolia ~ Sundews. About 8 bucks for 80 pellets.
It’s funny how my son and I have been immunized, everyone I know has been immunized and not one of us has ever had whooping cough. Herbs do not cure or prevent whooping cough. IMMUNIZE your kids. It is irresponsible not to.
On another note, it is just plain annoying that people like you seem to think you know more than scientists. That is also irresponsible.
Hi Kelly! I’m so sorry you’ve been annoyed enough to take time out of your day to comment on my blog. Thankfully, you seem to have saved time by not actually reading the post. 🙂 If you had read the post, you’d see that my kids were also immunized for whooping cough. And that only one strain of whooping cough is targeted with immunization. And that all of the information I’ve shared in this series is backed up by links to articles written by the CDC or clinical textbooks.
I feel certain that we differ on our stance on medical choice as well, and that parents should have the right to make informed medical decisions for their children. In a way, I feel for you, because (aside from the aggression and interest in other’s choices) I was in your shoes when I was a new mother, and trusted the pediatricians to know more than I did. Life taught me some hard lessons that I hope you don’t have to learn.
Hi Gwen,
How long did it take for your baby to recover fully ie no more coughing? Did he catch a cold in the 6-9 months after recovery? How is his health now?
My youngest one took about 5 weeks to be cough free, which is a lot shorter than it took for older kids, since we didn’t realize what was going on for a couple months with them. Their coughs were so sporadic and they seemed perfectly healthy between coughing spells. Also, some cases the cough is fairly mild, and even mine with the more forceful coughs weren’t whooping with them.
It took about 3 months for my oldest kids to stop coughing. My youngest guy is perfectly fine now. He’s now 6 years old, and is rarely sick. He does not have weak lungs.
I have a friend whose child has weaker lungs, and colds and infections always seem to migrate there. She had great success with a child friendly herbal tincture called Asma from Trilight Herbs. That’s what I’d try if my child seemed to have weak lungs.
Hi Gwen thank you so much for taking time to answer my question. Really appreciate it.
Just to clarify. Is it 5 weeks & 3 months of recovery stage or from the onset of the cough? Other than the syrup and the stew were there anything you did to speed up recovery?
How does one know if a child is in recovery stage? They are only considered recovered once coughing stops? Will they ever stop coughing?
Thanks again Gwen. Am very glad to hear that your little guy is perfectly healthy now and he is 6!
Such a nice reply. I love when people keep their cool in the face of criticism. <3 I've read and reread this post (and parts II and III). I can't tell you how it's eased my mind in the face of myself, my immunized 4yo, and my non immunized 1yo. We've all had/have it, I am almost 100%. Incorporating lots of natural tools, but just grateful to hear such excellent research and documented personal experience.
Hi Gwen~
I just came across This Very Interesting Topic in your blog… I just wanted to tell You that: Kelly WAS RESPONDING TO PATRICK’S POST~ NOT What YOU Wrote (Patrick is ONE OF THOSE PEOPLE Who BELIEVE That ALL HORRIBLE & HIGHLY CONTAGIOUS DISEASES Can Be Cured/Be Automatically Immunized To The Body WITH HERBS & ORGANIC FOOD… OH YEAH, AND CLEAN WATER! OMG, Seriously.
Anyway, I cannot even begin to get into THAT Topic. And my task & concern was to help you understand what The Chain Of Events Are here! You are SO smart & driven in your need to do research so YOU KNOW WHAT’S GOING ON & HOW YOU CAN PROTECT YOUR MUNCHKINS~ SMALL AAAND LARGE!
I was simply looking at THAT FABBY BBQ CHICKEN RECIPE, And A.D.D. Wandered Off To THE HORRIBLE WHOPPING COUGH STORY… YIKES!! In cases like This, AND PEOPLE LIKE PATRICK, I’m Somewhat Thankful I Don’t Have Kids (Until The Day I’ll Hopefully Be Able~ IF I’m NOT Too Old, And Sick w/fibromyalgia~ To Foster and/or Adopt Children. It’s My Dream!)
Thanks For EVERYTHING YOU DO~ THE INCREDIBLE EFFORT YOU PUT FORTH ON YOUR BLOG~ IT’S ALL SO EXCELLENT. THANK YOU! Kat
Why you feel the need to chastise others for their personal choices about their family is beyond my comprehension. You obviously feel the need to push your “Rightness” on other people and it is childish and silly. Who are you to call this women irresponsible? If you don’t like what she has to say then don’t waste your time reading it and responding like you’re freaking queen bee. And obviously you did not read and comprehend the article because she clearly states that some of her children were vaccinated and got it anyway, so clearly you’re here just to make others feel small. GO AWAY YOU ASS-HAT!
And Gwen you go girl, we are having great success with your tips.
Previous comment was directed at Kelly M.
Agreed. My whole family has been vaccinated and never had whooping cough…
I really have to thank you for this article. I am currently in the throws of whooping cough. I had to take my littlest to the doctor three times before I *insisted* on seeing the actual doctor, they kept putting us with a nurse practitioner. My other son was with him from the second visit on.
I myself am now coughing terrible. I must look awful as I am so tired from either caring for them, or trying to care for myself. I cannot imagine in your story that you were preparing to go on vacation! I don’t know how you found the energy!
THANK YOU for letting me know what is actually happening within the body. I was not understanding. The coughing until they turn purple, yes, that is some scary stuff!
I will be making the cough syrup and adding the turmeric to things too! And the stew!
Hi Gwen
Such a relief to chance upon your site since there aren’t many blogs by parents on this whooping cough issue.
My 6 yr old is at 4th week of stage 2. Less coughing but cough intensity and occasional vomiting unchanged.
*Will there still be vomiting at stage 3?
* Any obvious signs she’s into stage 3?
* any tips for stage 3 in preventing lung reinfection or building up strong lungs again
Her 2.5 yr old sister was given antibiotics when we first spotted her coughing. Are you aware if she will also develop coughing fits? And if anyone in the childcare still carries the bacteria unknowingly, does the antibodies wear off so fast that results in her getting reinfection?
Appreciate your advice
I’m so sorry I missed your comment. I don’t have any clear answers to your questions, and by this time, it probably is a moot point. I’m just sharing my research and experience from our bout.
As far as I know, natural infection results in antibodies to that strain. I am not sure anyone truly knows how long natural immunity lasts. We’ve never had another round, and it’s been over a decade at this point.